by Amy Mullins, PhD, RDN | Nov 24, 2021
The holiday season is finally upon us. It’s a time for enjoying family, friends, and food!
You can make healthy habits this holiday season. It’s not only a single meal but rather an entire season of parties, events, gatherings festivities, and unhealthy choices that add up to that holiday weight gain we resolve to lose when January rolls around. As the holiday season begins its rapid approach, take time and consider those eating habits that set your new year off on the wrong foot. Why not make a resolution now to eat healthier this holiday season?
Just a few simple strategies can help make the difference and keep those unwanted pounds away. Here are some suggestions:
- Don’t skip meals. Eating healthy on a regular basis will keep you from overindulging at holiday gatherings.
- Use smaller plates for meals and gatherings and be mindful of portions
- Choose more vegetables and smaller helpings of entrees and desserts
- Drink more water and minimize alcoholic drinks and eggnog
- Make healthier recipe ingredient substitutions when cooking and baking
Take a mindful approach to keeping your personal health goals in-check. We can all still experience the joy of the holiday season, without making food the focus. Make a resolution to be mindful and eat healthier this holiday season, and your waistline will thank you!
 Learn more about making healthy habits this holiday season!
Learn more about making healthy habits this holiday season!
— Tips for Making Healthy Choices
— Simple Substitutions
— Diabetes During the Holidays
— How to Add Fruits and Veggies
— Cranberry Nutrition
— Cranberry Sauce Recipe
— Holiday Food Safety Tips
Click here to read the newsletter.

by Amy Mullins, PhD, RDN | Nov 23, 2021
 Take care of your bones today for better quality of life tomorrow!
Take care of your bones today for better quality of life tomorrow!
According to the National Institutes of Health, about one in every two Americans over the age of 50 may already have or be at risk of developing osteoporosis. (1) Osteoporosis is a disease where, over time, bone quality and strength decline, making bones more likely to fracture and break. Fractures can develop not only as a result of a slip or fall but also from everyday sneezing or coughing. If your doctor diagnoses you with osteoporosis, the best course of action for slowing its progression may be prescription medication. However, nutrition and exercise can help provide a good foundation to prevent or delay disease development. (1)
Know Your Risks
While all risks are not completely understood, there is a genetic factor linked to osteoporosis – mainly, if poor bone mineral density runs in the family. In addition to genetic factors, poor nutrition, smoking, excessive alcohol, and a lack of exercise can all increase your risk of developing osteoporosis. It is important to talk to your doctor to discuss your level of risk and prevention measures. (1)
Build More Bone
Although they may not seem like it, bones are a living tissue and go through times of building and breakdown during the life cycle. Bones grow the most during childhood, but they also change and become stronger as an adult by doing exercises like weightlifting or running. (1) Similar to a savings account or retirement fund, the more you build when you are young, the more you can afford to spend as you age. Current recommendations to support strong bones include muscle strengthening exercises at least two times per week. These exercises require your muscles to do more work than doing just day-to-day activities. Additionally, strength training exercises should be done to the point where it would be difficult to perform one or two more repetitions. Examples include lifting weights, working with resistance bands, and doing body weight exercises such as push-ups, pull-ups, and planks. Additionally, climbing stairs, and carrying heavy loads (such as groceries and heavy gardening) also count when done frequently.(2)
Support Your Bones
In addition to exercise, nutrition plays a large role in promoting healthy bones. The two most important nutrients for bone health are calcium and vitamin D. Calcium is what gives bones their strength but is also involved in many other processes in the body. If you do not regularly consume enough calcium, your body takes it from your bones. (3) If this happens for long enough, your bones will become weakened and begin to develop osteoporosis. Vitamin D is important for the absorption of calcium. Not having enough vitamin D can impact your bones, even if you get enough calcium from your diet. (4)
| Life-stage group |
Calcium (mg/day) |
Vitamin D (IU/day) |
| Infants 0-6 months |
200 |
400 |
| Infants 6-12 months |
260 |
400 |
| 1-3 years old |
700 |
600 |
| 4-8 years old |
1,000 |
600 |
| 9-13 years old |
1,300 |
600 |
| 14-18 years old |
1,300 |
600 |
| 19-30 years old |
1,000 |
600 |
| 31-50 years old |
1,000 |
600 |
| 51–70-year-old males |
1,000 |
600 |
| 51–70-year-old females |
1,200 |
600 |
| > 70 years old |
1,200 |
600 |
| 14-18 years old, pregnant/lactating |
1,300 |
600 |
| 19-50 years old, pregnant/lactating |
1,000 |
600 |
Recommended Calcium and Vitamin D Intakes (5) Definitions: mg = milligrams; IU = International Units
Bone Strengthening Foods
There are a variety of food sources that provide calcium and vitamin D. Calcium can be found in dairy products, green vegetables, and calcium-fortified foods. Examples of calcium-containing dairy products include cheese, yogurt, and reduced-fat milk. Other calcium-fortified foods include breads, orange juice, cereals, and tofu. When it comes to vitamin D in your diet, be sure to include fatty fish such as tuna and salmon. There are smaller amounts of vitamin D found in cheese, mushrooms, and beef liver. Similar to calcium, there are many vitamin D-fortified foods available. Some examples are cereals, orange juice, milk, and milk products. Check out the two tables below for calcium and vitamin D food sources. (5)
Calcium Content of Selected Foods
| Food |
Serving size |
Milligram (mg) per serving |
% DV |
| Sardines, canned in oil |
3 oz |
324 |
32% |
| Cheddar cheese, shredded |
1 ½ oz |
306 |
31% |
| Nonfat milk |
8 oz |
302 |
30% |
| Yogurt, reduced fat, no solids |
8 oz |
300 |
30% |
| 2% milk (reduced fat) |
8 fl oz |
297 |
30% |
| Whole milk |
8 fl oz |
291 |
29% |
| Cottage cheese, 1% milk fat |
2 cups, unpacked |
276 |
28% |
| Mozzarella, part skim |
1 ½ oz |
275 |
28% |
| Tofu firm, with calcium |
½ cup |
204 |
20% |
| Orange juice, calcium fortified |
6 fl oz |
200-260 |
20-26% |
| Tofu soft, with calcium |
½ cup |
138 |
14% |
| Frozen yogurt, vanilla, soft serve |
½ cup |
103 |
10% |
| Ready-to-eat cereal, calcium fortified |
1 cup |
100-1000 |
10-100% |
| Turnip greens, boiled |
½ cup |
99 |
10% |
| Kale, raw |
1 cup |
90 |
9% |
| Vanilla ice cream |
½ cup |
85 |
8.5% |
| Soy beverage, calcium fortified |
8 fl oz |
80-500 |
8-50% |
| Flour tortilla |
1, 6” diameter |
37 |
4% |
| Sour cream, reduced fat, cultured |
2 Tbsp |
32 |
3% |
Adapted from Office of the Surgeon General (US). Bone Health and Osteoporosis: A Report of the Surgeon General. (7)
Vitamin D Content of Selected Foods
| Food |
Serving size |
Micrograms (mcg) per serving |
International Units (IU) per serving |
Percent DV |
| Cod liver oil |
1 Tbsp |
34 |
1,360 |
170 |
| Rainbow trout, cooked |
3 oz |
16.2 |
645 |
81 |
| Salmon (sockeye), cooked |
3 oz |
14.2 |
570 |
71 |
| White mushrooms, raw, exposed to UV light |
½ cup |
9.2 |
366 |
46 |
| 2% milk, vitamin D fortified |
1 cup |
2.9 |
120 |
15 |
| Soy, almond, & oat milk, vitamin D fortified |
1 cup |
2.5-3.6 |
100-144 |
13-18 |
| Ready-to-eat cereal, fortified with 10% DV vitamin D |
1 serving |
2.0 |
80 |
10 |
| Sardines (Atlantic), canned in oil, drained |
2 |
1.2 |
46 |
6 |
| Egg, scrambled |
1 large |
1.1 |
44 |
6 |
| Beef liver, braised |
3 oz |
1.0 |
42 |
5 |
| Tuna fish (light), canned in water, drained |
3 oz |
1.0 |
40 |
5 |
| Cheddar cheese |
1.5 oz |
0.4 |
17 |
2 |
| Portabella mushrooms, raw, diced |
½ cup |
0.1 |
4 |
1 |
| Chicken breast, roasted |
3 oz |
0.1 |
4 |
1 |
| Ground beef, 90% lean, broiled |
3 oz |
0 |
1.7 |
0 |
| Broccoli, raw, chopped |
½ cup |
0 |
0 |
0 |
Adapted from Vitamin D – Fact sheet for health professionals (8)
Stay Safe and Healthy as You Age
Osteoporosis can be a serious and life changing diagnosis. However, adopting healthy habits like limiting smoking and excessive alcohol consumption can decrease your risk. Consuming enough calcium and vitamin D each day and getting regular muscle building exercise at least twice a week can also help protect your bones. Women over the age of 65, or anyone diagnosed as “at risk,” should be regularly screened for osteoporosis by a doctor during their yearly physical health exam. (6,7,8)
Making healthy lifestyle choices from a young age can help prevent or delay osteoporosis, but once you’re diagnosed, the best course of action for slowing its progression may be prescription medication. Consult your doctor before beginning a new exercise program or for interactions with medications.
References
- “Osteoporosis Overview.” National Institutes of Health, U.S. Department of Health and Human Services, https://www.bones.nih.gov/health-info/bone/osteoporosis/overview.
- S. Department of Health and Human Services. Physical Activity Guidelines for Americans, 2nd edition. Washington, DC: U.S. Department of Health and Human Services; 2018.
- “Osteoporosis.” Edited by Susan Randall, Osteoporosis | Office on Women’s Health, National Institute of Arthritis and Musculoskeletal and Skin Diseases, 20 May 2019, https://www.womenshealth.gov/a-z-topics/osteoporosis.
- “Office of Dietary Supplements – Vitamin D.” NIH Office of Dietary Supplements, U.S. Department of Health and Human Services, 22 Mar. 2021, https://ods.od.nih.gov/factsheets/vitaminD-HealthProfessional/
- S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020-2025. 9th Edition. December 2020. Available at DietaryGuidelines.gov
- Palmer S. Bone Health and Diet. Today’s Dietitian. 2013;15(2):44.
- Office of the Surgeon General (US). Bone health and osteoporosis: A report of the surgeon general. Rockville (MD): Office of the Surgeon General (US); 2004. Table 7-2, Selected Food Sources of Calcium. Available from: https://www.ncbi.nlm.nih.gov/books/NBK45523/table/ch7.t2/
- Vitamin D – Fact sheet for health professionals. NIH Office of Dietary Supplements. https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/#h3. Published August 17, 2021. Accessed November 11, 2021.
Guest contributors: Andrew Treble and Lexi Fraino are master’s students and Dietetic Interns from Florida State University’s Department of Nutrition & Integrative Physiology.
by Heidi Copeland | Nov 23, 2021
Since I can recall, I’ve liked to read cookbooks. Old cookbooks, famous cookbooks, church cookbooks, regional and seasonal cookbooks, and cookbooks hot off the press! I read the forward and the preface (… if there is one). I don’t just look at the pictures, but I read the recipe for yield (number of servings), ingredients and amounts, and the way the ingredients are combined. I read about the equipment required to prepare the recipe and the amount of time it takes to complete the task.
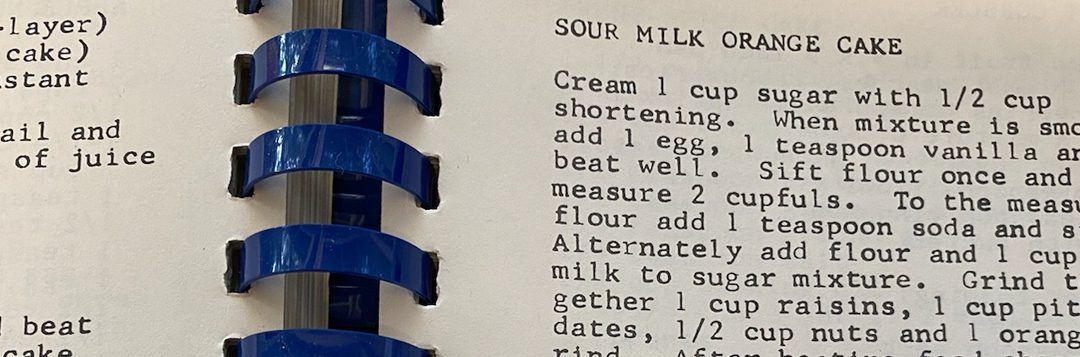
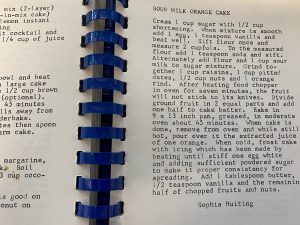
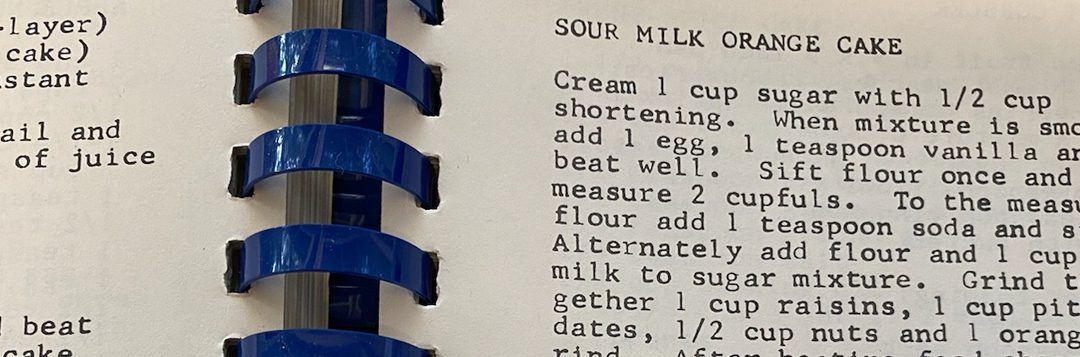
A narrative format is common with many older or handwritten recipes.
Photo credit: Heidi Copeland
Generally, I have found that old cookbook recipes often seem different and that handwritten, handed-down recipes tend to be vague. I also have found that the product does not always turn out like the picture. Yields – the amount a recipe feeds – has certainly changed over time and recipe ingredients have become more and more varied, as has their use. Who knew toasting spices completely changes their flavor profile and that umami is important?
It used to be that people learned to cook by watching someone else. However, that seriously changed as more and more folks became literate. In fact, the first cookbook published in the United States, American Cookery (Hartford Connecticut 1796), has been designated by The Library of Congress as one of the 88 books that shaped America. This first cookbook used uniquely American ingredients of the time and provided American cooks with quite a litany of receipts, the old-world way of documenting what we now call a recipe.
Recently, I listened to a radio interview with Adrien Miller, a cookbook author who has been on a quest to document uniquely African American cooking histories.
I chuckled to hear Adrien Miller describe a handwritten recipe from a friend or a relative as a lesserpe… his terminology for the unexacting nature of a recipe given from someone who really doesn’t need an exact rendition because they know what they are doing and assume you do, too.
Recipes are a great way to hand down our own historical traditions. However, having been charged with giving out a lesserpe…, I find it is critically important to be as exacting as possible when sharing recipes with friends or family.
A good, standard format for a recipe includes:
- Name of product
- Yield of product (how many it serves)
- Ingredients in exact amounts (in order of use is helpful)
- Step-by-step instructions, in detail
- Time and temperature specifics
- Important information about pan size, etc.
Remember, too, that a recipe is a history. History evolves. Aunt Margaret might have written a narrative format (paragraph) recipe but today that form might be seen as hard to follow.
Here is an example from Aunt Margaret:
Apple Pie (2 crust)
Preheat oven to 425 degrees. Line a 9-inch pie pan with your favorite crust. Combine and sift together 1/2 – 2/3 cup white sugar, 1 1/2 tablespoons cornstarch, 1/4 teaspoon nutmeg, 1/2 teaspoon cinnamon. Combine and sift over apples (about 3#, cut up). Stir apples gently until well coated. Place in pie shell and dot with butter. Cover pie, slit or prick crust. Bake at 425 degrees for about 15 minutes then reduce heat to 375 degrees. Bake until done.
The typically formatted recipe:
Apple Pie (Aunt Margaret)
Serves 8 to 10
2 pie crusts, purchased or homemade
3 pounds Granny Smith apples, approximately 8 large apples
1/2 cup white sugar, more if you like it sweeter
1 1/2 tablespoons cornstarch
1/4 teaspoon nutmeg
1/2 teaspoon cinnamon
2 tablespoons butter, firm, sliced thin
1 egg yolk
2 tablespoons cream
- Preheat oven to 425°F.
- Wash, peel, core, and slice the apples thinly.
- In a large bowl, toss sliced apples with sugar, cornstarch, nutmeg, and cinnamon.
- Line 9” pie pan with 1 piecrust
- Mound the apple mixture in the center of the pie crust.
- Dot the apple mixture with sliced butter.
- Cover apples with 2nd pie crust.
- Crimp edges of the pie crust. (Press the top and bottom dough rounds together as you flute edges using thumb and forefinger or press with a fork.)
- Mix egg yolk and cream, brush all over the pie crust top.
- Stick with fork tines in a dozen places or vent with small knife-made slits.
- Bake 15 minutes in the preheated 425°oven.
- Reduce the temperature to 375°. Continue baking for 35 to 45 minutes, until apples are soft and the crust is golden brown.
- Transfer the apple pie to a rack to cool for at least 1 hour.
- Serve warm or cold.
Notes:
- Place the pie on a baking sheet to catch any drips before you bake it.
- At any point during the baking, if the top of the pie begins to brown too much, just tent it with aluminum foil.
- Your dad does not like nutmeg. I add a splash of vanilla, a bit more cinnamon, and omit the nutmeg.
- Don’t forget the vanilla bean ice-cream. It adds a nice touch!
This holiday season, don’t be blamed for sharing less than the whole recipe. Recipes can be a valuable tool for passing on important family food traditions, now and into the distant future. Learn to write a good recipe with details. You might just be the talk of the table for eons.
Library of Congress: American Cookery
by Claire Davis | Oct 26, 2021

Photo Source: Auburn University IHSA Equestrian Team
Claire Reach is the UF/IFAS 4-H & Family and Consumer Sciences (FCS) Agent in Calhoun County, Florida. For 4-H, she specializes in animal handling, animal safety, and animal sciences. For FCS, she mainly specializes in food safety and healthy living, but has found a new opportunity to work with First Time Homebuyers and the State Housing Initiative Partnership Program (SHIP) in the county.
Claire grew up in Alabama, splitting her time between Birmingham and her family’s farm, L & L Angus Farm, in Auburn. The family farm is Claire’s driving force behind the passion that she has for agriculture, which is a large part of the work she is doing in Extension.

These pictures are of my family on the farm in Auburn, AL. Photo Source: Dave Davis.

Peep some of the cows in the background. Photo Source: Elise Reach.
With a family background in Ag, she decided to study Animal Science-Production Management at Auburn University in Auburn, Alabama. While completing her undergraduate degree, Claire competed for Auburn University’s Intercollegiate Horse Show Association, worked at Auburn University’s College of Veterinary Medicine in a research barn, and continued to work on the family farm. She graduated in May of 2019 with her Bachelor of Science and a minor in Agricultural Business.

Several home cooking/canning classes offered in 2021. Strawberry jam, chicken, pepper jelly, salsa, and mozzarella cheese have been made! Photo Source: Claire Reach UF/IFAS.

The Calhoun County 4-H Horse Club recently started up! (The 2 horses on the right side of the image also belong to me.) Photo Source: Dave Davis.
Shortly after graduation, she moved to Florida to work for Deseret Cattle and Timber as a Heavy Machinery Operator, but soon realized that her passion was Extension. The position in Calhoun County became available and she jumped at the opportunity to apply for it. Having just started in May 2021, Claire has not been with UF/IFAS Extension long, but she cannot wait to see what the future holds for her county. Claire says that she aspires for the Calhoun County FCS Program to be the area’s leading program for adults in practical home practices, whether that be home canning or healthy eating, and healthy living. All the programs that she offers, whether it be 4-H or FCS, follow the same motto: ‘learn by doing’. This drives the experience of each program, allowing participants to fully understand a concept or ask questions when they do not.

These are the “goodest” dogs of all time! Evie (Chocolate Lab), Diesel (Black and White Mutt), and Hank (Bassett Hound-laying down) Peep the chickens, turkeys, cat, and horses in the back ground! Photo Source: Claire Reach UF/IFAS.

This is Chick! For a mare, she’s pretty special. We have a great bond and she trusts me to do just about anything with her (i.e. shoot a gun off of, rope cattle, stand on, lay on, or let little kids ride) Photo Source: Tanner Mayo.
When Claire is not at work, she says there is always more work to be done at home. Living on a functioning livestock operation, she has several animals, including: chickens (about 50 at the moment), 5 guineas, 4 turkeys, 2 cats, 4 dogs, and 3 horses. She hopes to be able to add cattle to the ever-growing “funny farm” soon! It isn’t always about work, though. In her spare time, Claire enjoys spending time with family, riding her horses, long walks with the dogs, dirt road riding, and paddle boarding at the beach!

by Samantha Kennedy | Oct 26, 2021
If baking were a feature film, flour would be the lead actor. While there are a lot of important supporting castmates, flour is the star. It serves as the foundation upon which baking masterpieces are built, providing structure, texture, and mouthfeel (the physical sensations food provides in the mouth) to the final product.
But here is the thing: Not all flours are created equal. There are many types of flour out there, but not all of them will provide the same results. Different types of flour have different levels of protein, gluten, and fiber, and react differently with their companion ingredients. Need all-purpose flour but only have rye flour? Expect a nuttier, grainier outcome – or even possibly a disaster!
Depending on the type of flour used, different quantities of other ingredients may be called for, such as water or oil, salt, butter, sugar, baking soda, or baking powder. Not all flours are easily interchangeable, and some flours can only be partially substituted for others, or the final product may be dramatically different.
For example, want to substitute whole wheat flour for all-purpose flour? Sure, it’s possible, and is much easier to pull off in quick (non-yeast) breads such as muffins, pancakes, and biscuits. However, in yeast breads, switching out 100% of white flour for whole wheat without adjusting other ingredients will inevitably result in a final product that is less airy and more dense (less rise), which may adversely affect the flavor and texture.
What to do? Since whole wheat flour absorbs more liquid than white flour, for every 1 cup of whole wheat flour substituted, increase the liquid by 2 teaspoons, and then let the dough rest for 30 minutes before kneading to allow the liquid to be absorbed. This will result in a softer, more malleable dough that will yield more favorable final results.
There are many more substitution tips out there – more than could possibly be covered in one article. But here are a few common types of flour that may be called for in baking:

All-purpose flour is a common, highly versatile type of flour that can be used successfully in many baking recipes. (Source: Samantha Kennedy)
All-purpose flour: Made from the soft, chewy internal part of the wheat kernel – the endosperm – it is a highly versatile type of flour that can be used in just about any baking recipe. This type of flour generally contains about 10-11% protein.
Self-rising flour: I like to think of this as all-purpose flour with a kick. Why? Because it already contains the salt and baking powder that would otherwise need to be added to all-purpose flour to make the final product rise. While it can be substituted for all-purpose flour, it is important to remember to leave out the additional salt and baking powder called for in the recipe.
Bread flour: This type of flour has a higher protein content than all-purpose flour – about 12% – and produces a dough with more gluten, resulting in a light, airy loaf with good volume. All-purpose flour can be used instead with positive results.
Cake flour: This type of flour contains about 7.5% protein and results in a final product that is crumblier than bread, which is desirable in a cake or cupcake. If using all-purpose flour instead, substitute 1 cup minus 2 tablespoons of all-purpose flour for every 1 cup of cake flour called for in the recipe.
Flour is a vital ingredient in nearly all baked goods. Using too much, too little, or a different kind than called for can result in an unsatisfactory final product. Learning the differences between common types of flour and how they can be interchanged with one another will go a long way towards achieving baking success.
For more information about this or other baking topics, please call Samantha Kennedy at (850) 926-3931.
UF/IFAS is an Equal Opportunity Institution.

by Judy Corbus | Oct 22, 2021

Consider setting up a flexible spending account during your employer’s open enrollment period. Photo credit: Judy Corbus
Fall is open enrollment for health insurance and other employee benefits with many employers. One benefit available through many employers is a flexible spending account, or FSA. A flexible spending account is a special account into which you put money to pay for certain out-of-pocket health care expenses. You select the total amount you wish to contribute for the following year, and your contributions are divided out evenly over your paycheck schedule beginning January 1st.
A real perk to this account is you don’t pay taxes on your contributions – the money is deducted before taxes are calculated so you will save an amount equal to the taxes you would have paid on the money you have set aside.
The FSA funds can be used to pay for certain medical and dental expenses for you, your spouse if you’re married, and your dependents. Typical allowable expenses include:
- Deductibles and co-payments
- Prescription medications and over-the-counter medications with a doctor’s prescription
- Medical supplies and equipment such as crutches, bandages, contact lenses and solution, hearing aid batteries, and blood sugar test kits.
Access to your funds varies by employer – some provide employees with a special debit card linked to their FSA to use to pay for expenses, while others require employees to submit a claim to the FSA for reimbursement.
You may contribute a maximum of $2,750 per year per employer. Your spouse also may contribute up to $2,750 in an FSA with their employer. Bear in mind that FSAs are “use it or lose it.” Funds generally must be used within the plan year; however, employers may offer a couple of options:
- They may provide a “grace period” of up to 2 ½ extra months to use the funds.
- They may allow you to carry over up to $550 per year to use in the following year.
Employers are not required to offer these options so it’s important to know your employer’s policy. If you have not used your money by the end of the plan year or grace period, you lose it so plan carefully.
To calculate how much to contribute, review this year’s medical expenses for routine doctor and dentist visit co-pays and charges, deductibles, prescription and OTC “maintenance” medications, and other medical expenses. If you anticipate an additional expense for the coming year, such as new eyeglasses, factor that in as well. It’s better to underestimate next year’s medical expenses and contribute a smaller amount than to overestimate and risk losing unused funds.
Some employers also offer dependent care flexible spending accounts to cover childcare expenses. They, too, offer tax savings and operate similarly to healthcare FSAs; check with your employer to see if they are available.
Use open enrollment to review your available options and premiums and compare with your current plan(s) to make sure you and your family are enrolled in the plan(s) that will best meet your needs at the most affordable price. Consider enrolling in a flexible spending account to save money on taxes – don’t leave money on the table!
For more information, visit IRS Publication 969 Health Savings Accounts and Other Tax-Favored Health Plans.
Source: HealthCare.gov

 Learn more about making healthy habits this holiday season!
Learn more about making healthy habits this holiday season!